- Record: found
- Abstract: found
- Article: found
Comparison of cardiovascular magnetic resonance characteristics and clinical consequences in children and adolescents with isolated left ventricular non-compaction with and without late gadolinium enhancement
Read this article at
Abstract
Background
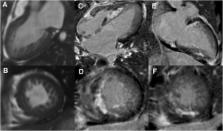
Although cardiovascular magnetic resonance (CMR) is showing increasingly diagnostic potential in left ventricular non-compaction (LVNC), relatively little research relevant to CMR is conducted in children with LVNC. This study was performed to characterize and compare CMR features and clinical outcomes in children with LVNC with and without late gadolinium enhancement (LGE).
Methods
A cohort of 40 consecutive children (age, 13.7 ± 3.3 years; 29 boys and 11 girls) with isolated LVNC underwent a baseline CMR scan with subsequent clinical follow-up. Short-axis cine images were used to calculate left ventricular (LV) ejection fraction (EF), end-diastolic volume (EDV), end-systolic volume (ESV), myocardial mass, ratio of non-compacted-to-compacted myocardial thickness (NC/C ratio), and number of non-compacted segments. The LGE images were analyzed to assess visually presence and patterns of LGE. The primary end point was a composite of cardiac death and heart transplantation.
Results
The LGE was present in 10 (25 %) children, and 46 (27 %) segments were involved, including 23 non-compacted segments and 23 normal segments. Compared with LGE- cohort, LGE+ cohort had significantly lower LVEF (23.8 ± 10.7 % vs. 42.9 ± 16.7 %, p < 0.001) and greater LVEDV (169.2 ± 65.1 vs. 118.2 ± 48.9 mL/m 2, p = 0.010), LVESV (131.3 ± 55.5 vs. 73.3 ± 46.7 mL/m 2, p = 0.002), and sphericity indices (0.75 ± 0.19 vs. 0.60 ± 0.20, p = 0.045). There were no differences in terms of number and distribution of non-compacted segments, NC/C ratio, and myocardial mass index between LGE+ and LGE- cohort. In the LGE+ cohort, adverse events occurred in 6 patients compared to 2 events in the LGE- cohort. Kaplan-Meier analysis showed a significant difference in outcome between LGE+ and LGE- cohort for cardiac death and heart transplantation ( p = 0.011).
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy.
- Record: found
- Abstract: found
- Article: not found
Isolated noncompaction of left ventricular myocardium. A study of eight cases.
- Record: found
- Abstract: found
- Article: not found