- Record: found
- Abstract: found
- Article: found
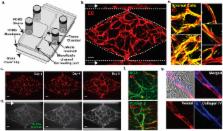
3D microtumors in vitro supported by perfused vascular networks
Read this article at
Abstract
There is a growing interest in developing microphysiological systems that can be used to model both normal and pathological human organs in vitro. This “organs-on-chips” approach aims to capture key structural and physiological characteristics of the target tissue. Here we describe in vitro vascularized microtumors (VMTs). This “tumor-on-a-chip” platform incorporates human tumor and stromal cells that grow in a 3D extracellular matrix and that depend for survival on nutrient delivery through living, perfused microvessels. Both colorectal and breast cancer cells grow vigorously in the platform and respond to standard-of-care therapies, showing reduced growth and/or regression. Vascular-targeting agents with different mechanisms of action can also be distinguished, and we find that drugs targeting only VEGFRs (Apatinib and Vandetanib) are not effective, whereas drugs that target VEGFRs, PDGFR and Tie2 (Linifanib and Cabozantinib) do regress the vasculature. Tumors in the VMT show strong metabolic heterogeneity when imaged using NADH Fluorescent Lifetime Imaging Microscopy and, compared to their surrounding stroma, many show a higher free/bound NADH ratio consistent with their known preference for aerobic glycolysis. The VMT platform provides a unique model for studying vascularized solid tumors in vitro.
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
Improved survival with bevacizumab in advanced cervical cancer.

- Record: found
- Abstract: found
- Article: found