- Record: found
- Abstract: found
- Article: found
Effects of dexmedetomidine on oxygenation and lung mechanics in patients with moderate chronic obstructive pulmonary disease undergoing lung cancer surgery : A randomised double-blinded trial
Read this article at
Abstract
BACKGROUND
Chronic obstructive pulmonary disease (COPD) is a risk factor that increases the incidence of postoperative cardiopulmonary morbidity and mortality after lung resection. Dexmedetomidine, a selective α 2-adrenoreceptor agonist, has been reported previously to attenuate intrapulmonary shunt during one-lung ventilation (OLV) and to alleviate bronchoconstriction.
OBJECTIVE
The objective is to determine whether dexmedetomidine improves oxygenation and lung mechanics in patients with moderate COPD during lung cancer surgery.
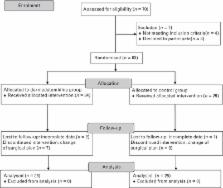
PARTICIPANTS
Fifty patients scheduled for video-assisted thoracoscopic surgery who had moderate COPD. Patients were randomly allocated to a control group or a Dex group ( n = 25 each).
INTERVENTIONS
In the Dex group, dexmedetomidine was given as an initial loading dose of 1.0 μg kg −1 over 10 min followed by a maintenance dose of 0.5 μg kg −1 h −1 during OLV while the control group was administered a comparable volume of 0.9% saline. Data were measured at 30 min (DEX-30) and 60 min (DEX-60) after dexmedetomidine or saline administration during OLV.
MAIN OUTCOME MEASURES
The primary outcome was the effect of dexmedetomidine on oxygenation. The secondary outcome was the effect of dexmedetomidine administration on postoperative pulmonary complications.
RESULTS
Patients in the Dex group had a significantly higher PaO 2/F iO 2 ratio (27.9 ± 5.8 vs. 22.5 ± 8.4 and 28.6 ± 5.9 vs. 21.0 ± 9.9 kPa, P < 0.05), significantly lower dead space ventilation (19.2 ± 8.5 vs. 24.1 ± 8.1 and 19.6 ± 6.7 vs. 25.3 ± 7.8%, P < 0.05) and higher dynamic compliance at DEX-30 and DEX-60 ( P = 0.0001 and P = 0.0184) compared with the control group. In the Dex group, the PaO 2/F iO 2 ratio in the postoperative period was significantly higher ( P = 0.022) and the incidence of ICU admission was lower than in the control group.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Hypoxic pulmonary vasoconstriction: physiology and anesthetic implications.
- Record: found
- Abstract: found
- Article: not found
Operative mortality and respiratory complications after lung resection for cancer: impact of chronic obstructive pulmonary disease and time trends.
- Record: found
- Abstract: found
- Article: not found