- Record: found
- Abstract: found
- Article: found
Adjunctive Use of Ketamine for Benzodiazepine-Resistant Severe Alcohol Withdrawal: a Retrospective Evaluation
Read this article at
Abstract
Introduction
Benzodiazepine (BZD)-resistant alcohol withdrawal remains a challenge for most institutions due to limited evidence with available agents. One published study currently exists utilizing the N-methyl- d-aspartate antagonist, ketamine, for alcohol withdrawal.
Objective
The purpose of our study was to evaluate the effect of adjunctive ketamine continuous infusion on symptom control and lorazepam infusion requirements for BZD-resistant alcohol withdrawal patients in the intensive care unit.
Methods
A retrospective review was conducted of patients receiving ketamine adjunctively with a lorazepam infusion for severe alcohol withdrawal between August 2012 and August 2014. Outcomes included time to symptom control, lorazepam infusion requirements, ketamine initial and maximum daily infusion rates, and adverse effects of ketamine.
Results
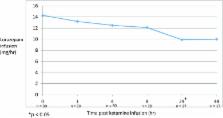
Thirty patients were included in the analysis. Mean time to initiation of ketamine after the initiation of a lorazepam infusion was 41.4 h. All patients achieved initial symptom control within 1 h of ketamine initiation. Median initial ketamine infusion rate was 0.75 mg/kg/h and the average maximum daily rate was 1.6 mg/kg/h. Significant decreases in lorazepam infusion rates from baseline were observed at 24 h (− 4 mg/h; p = 0.01) after ketamine initiation. No patients experienced documented CNS adverse effects. Two patients experienced hypertension and no patients experienced tachycardia related to ketamine.
Conclusion
Adjunctive ketamine could provide symptom control for BZD-refractory patients and may potentially reduce lorazepam infusion requirements. Future studies to determine optimal dosing, timing of initiation, and place in therapy for BZD-resistant alcohol withdrawal are needed. The mechanism of action via the NMDA receptor with ketamine may provide benefit for BZD-resistant alcohol withdrawal.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: found
Ketamine: Current applications in anesthesia, pain, and critical care
- Record: found
- Abstract: found
- Article: not found
Alcohol withdrawal syndrome.
- Record: found
- Abstract: found
- Article: not found
