- Record: found
- Abstract: found
- Article: found
Disparities in Incidence of COVID-19 Among Underrepresented Racial/Ethnic Groups in Counties Identified as Hotspots During June 5–18, 2020 — 22 States, February–June 2020
research-article
Jazmyn T. Moore , MSc, MPH
1 ,
Jessica N. Ricaldi , MD, PhD
1
,
,
Charles E. Rose , PhD
1 ,
Jennifer Fuld , PhD
1 ,
Monica Parise , MD
1 ,
Gloria J. Kang , PhD
1 ,
Anne K. Driscoll , PhD
1 ,
Tina Norris , PhD
1 ,
Nana Wilson , PhD
1 ,
Gabriel Rainisch , MPH
1 ,
Eduardo Valverde , DrPH
1 ,
Vladislav Beresovsky , PhD
1 ,
Christine Agnew Brune , PhD
1 ,
Nadia L. Oussayef , JD
1 ,
Dale A. Rose , PhD
1 ,
Laura E. Adams , DVM
1 ,
Sindoos Awel
1 ,
Julie Villanueva , PhD
1 ,
Dana Meaney-Delman , MD
1 ,
Margaret A. Honein , PhD
1 ,
COVID-19 State, Tribal, Local, and Territorial Response Team
COVID-19 State, Tribal, Local, and Territorial Response Team
COVID-19 State, Tribal, Local, and Territorial Response Team
Gregory Bautista ,
Janet Cowins ,
Charles Edge ,
Gail Grant ,
Robbie Gray ,
Sean Griffing ,
Nikki Hayes ,
Laura Hughes ,
Rene Lavinghouze ,
Sarah Leonard ,
Robert Montierth ,
Krishna Palipudi ,
Victoria Rayle ,
Andrew Ruiz ,
Malaika Washington ,
Sherri Davidson ,
Jennifer Dillaha ,
Rachel Herlihy ,
Carina Blackmore ,
Thomas Troelstrup ,
Laura Edison ,
Ebony Thomas ,
Caitlin Pedati ,
Farah Ahmed ,
Catherine Brown ,
Sarah Lyon Callo ,
Kathryn Como-Sabetti ,
Paul Byers ,
Victor Sutton ,
Zackary Moore ,
Sietske de Fijter ,
Alexia Zhang ,
Linda Bell ,
John Dunn ,
Stephen Pont ,
Keegan McCaffrey ,
Emily Stephens ,
Ryan Westergaard
21 August 2020
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
During January 1, 2020–August 10, 2020, an estimated 5 million cases of coronavirus
disease 2019 (COVID-19) were reported in the United States.* Published state and national
data indicate that persons of color might be more likely to become infected with SARS-CoV-2,
the virus that causes COVID-19, experience more severe COVID-19–associated illness,
including that requiring hospitalization, and have higher risk for death from COVID-19
(
1
–
5
). CDC examined county-level disparities in COVID-19 cases among underrepresented
racial/ethnic groups in counties identified as hotspots, which are defined using algorithmic
thresholds related to the number of new cases and the changes in incidence.
†
Disparities were defined as difference of ≥5% between the proportion of cases and
the proportion of the population or a ratio ≥1.5 for the proportion of cases to the
proportion of the population for underrepresented racial/ethnic groups in each county.
During June 5–18, 205 counties in 33 states were identified as hotspots; among these
counties, race was reported for ≥50% of cumulative cases in 79 (38.5%) counties in
22 states; 96.2% of these counties had disparities in COVID-19 cases in one or more
underrepresented racial/ethnic groups. Hispanic/Latino (Hispanic) persons were the
largest group by population size (3.5 million persons) living in hotspot counties
where a disproportionate number of cases among that group was identified, followed
by black/African American (black) persons (2 million), American Indian/Alaska Native
(AI/AN) persons (61,000), Asian persons (36,000), and Native Hawaiian/other Pacific
Islander (NHPI) persons (31,000). Examining county-level data disaggregated by race/ethnicity
can help identify health disparities in COVID-19 cases and inform strategies for preventing
and slowing SARS-CoV-2 transmission. More complete race/ethnicity data are needed
to fully inform public health decision-making. Addressing the pandemic’s disproportionate
incidence of COVID-19 in communities of color can reduce the community-wide impact
of COVID-19 and improve health outcomes.
This analysis used cumulative county-level data during February–June 2020, reported
to CDC by jurisdictions or extracted from state and county websites and disaggregated
by race/ethnicity. Case counts, which included both probable and laboratory-confirmed
cases, were cross-referenced with counts from the HHS Protect database (https://protect-public.hhs.gov/).
Counties missing race data for more than half of reported cases (126) were excluded
from the analysis.
§
The proportion of the population for each county by race/ethnicity was calculated
using data obtained from CDC WONDER (
6
). For each underrepresented racial/ethnic group, disparities were defined as a difference
of ≥5% between the proportion of cases and the proportion of the population consisting
of that group or a ratio of ≥1.5 for the proportion of cases to the proportion of
the population in that racial/ethnic group. The county-level differences and ratios
between proportion of cases and the proportion of population were used as a base for
a simulation accounting for missing data using different assumptions of racial/ethnic
distribution of cases with unknown race/ethnicity. An intercept-only logistic regression
model was estimated for each race/ethnicity category and county to obtain the intercept
regression coefficient and standard error. The simulation used the logistic regression-estimated
coefficient and standard error to produce an estimated mean and confidence interval
(CI) for the percentage difference between and ratio of proportions of cases and population.
This simulation was done for each racial/ethnic group within each county. The lower
bound of the CI was used to identify counties with disparities (as defined by percentage
differences or ratio). The mean of the estimated differences and mean of the estimated
ratios were calculated for all counties with disparities. Analyses were conducted
using SAS software (version 9.4; SAS Institute).
During June 5–18, a total of 205 counties in 33 states were identified as hotspots.
These counties have a combined total population of 93.5 million persons, and approximately
535,000 cumulative probable and confirmed COVID-19 cases. Among the 205 identified
hotspot counties, 79 (38.5%) counties in 22 states, with a combined population of
27.5 million persons and approximately 162,000 COVID-19 cases, had race data available
for ≥50% of cumulative cases and were included in the analysis (range = 51.3%–97.4%).
Disparities in cases were identified among underrepresented racial/ethnic groups in
76 (96.2%) analyzed counties (Table 1). Disparities among Hispanic populations were
identified in approximately three quarters of hotspot counties (59 of 79, 74.7%) with
approximately 3.5 million Hispanic residents (Table 2). Approximately 2.0 million
black persons reside in 22 (27.8%) hotspot counties where black residents were disproportionately
affected by COVID-19, approximately 61,000 AI/AN persons live in three (3.8%) hotspot
counties where AI/AN residents were disproportionately affected by COVID-19, nearly
36,000 Asian persons live in four (5.1%) hotspot counties where Asian residents were
disproportionately affected by COVID-19, and approximately 31,000 NHPI persons live
in 19 (24.1%) hotspot counties where NHPI populations were disproportionately affected
by COVID-19.
TABLE 1
Total population and racial/ethnic disparities* in cumulative COVID-19 cases among
79 counties identified as hotspots during June 5–18, 2020, with any disparity identified
— 22 states, February–June 2020
State
No. of persons living in analyzed hotspot counties*
No. of (col %) hotspot counties analyzed†
No. of counties with disparities in COVID-19 cases among each racial/ethnic group§
Hispanic
Black
NHPI
Asian
AI/AN
Alabama
500,000–1,000,000
1 (1.3)
—
1
—
—
—
Arizona
1,000,000–3,000,000
5 (6.3)
3
—
—
—
3
Arkansas
500,000–1,000,000
4 (5.1)
4
—
2
—
—
California
1,000,000–3,000,000
1 (1.3)
1
—
—
—
—
Colorado
100,000–500,000
1 (1.3)
1
—
1
—
—
Florida
>3,000,000
6 (7.6)
3
2
—
—
—
Georgia
100,000–500,000
1 (1.3)
1
—
—
—
—
Iowa
50,000–100,000
1 (1.3)
1
—
—
—
—
Kansas
500,000–1,000,000
2 (2.5)
2
—
2
—
—
Massachusetts
500,000–1,000,000
2 (2.5)
—
2
—
—
—
Michigan
1,000,000–3,000,000
5 (6.3)
—
5
1
—
—
Minnesota
<50,000
1 (1.3)
1
1
1
1
—
Mississippi
100,000–500,000
2 (2.5)
1
2
—
—
—
North Carolina
>3,000,000
18 (22.8)
18
—
3
1
—
Ohio
1,000,000–3,000,000
3 (3.8)
3
2
—
1
—
Oregon
1,000,000–3,000,000
6 (7.6)
6
1
4
1
—
South Carolina
1,000,000–3,000,000
9 (11.4)
6
4
2
—
—
Tennessee
500,000–1,000,000
3 (3.8)
3
—
—
—
—
Texas
500,000–1,000,000
2 (2.5)
—
1
—
—
—
Utah
1,000,000–3,000,000
4 (5.1)
4
1
3
—
—
Virginia
<50,000
1 (1.3)
—
—
—
—
—
Wisconsin
100,000–500,000
1 (1.3)
1
—
—
—
—
Total (approximate)
27,500,000
79 (100)
59
22
19
4
3
Abbreviations: AI/AN = American Indian/Alaska Native; COVID-19 = coronavirus disease
2019; NHPI = Native Hawaiian/other Pacific Islanders.
* Disparities were defined as percentage difference of ≥5% between the proportion
of cases and the proportion of the population or a ratio ≥1.5 for the proportion of
cases to the proportion of the population) for underrepresented racial/ethnic groups
in each county.
† Counties with race/ethnicity data available for ≥50% of cases.
§ Racial/ethnic groups are not mutually exclusive in a given county.
TABLE 2
Number of persons in each racial/ethnic group living in 79 counties identified as
hotspots during June 5–18, 2020 with disparities* — 22 states, February–June 2020
Racial/Ethnic group
No. (%)† of counties with disparities§ identified
Approximate no. of persons living in hotspot counties with disparities
Hispanic/Latino
59 (74.7)
3,500,000
Black/African American
22 (27.8)
2,000,000
American Indian/Alaska Native
3 (3.8)
61,000
Asian
4 (5.1)
36,000
Native Hawaiian/Other Pacific Islander
19 (24.1)
31,000
Total
—
5,628,000
Abbreviation: COVID-19 = coronavirus disease 2019.
* Disparities were defined as percentage difference of ≥5% between the proportion
of cases and the proportion of the population or a ratio ≥1.5 for the proportion of
cases to the proportion of the population) for underrepresented racial/ethnic groups
in each county.
†
Percentage of the 79 counties.
§ Disparities are in respective racial/ethnic groups and are not mutually exclusive;
some counties had disparities in more than one racial/ethnic group.
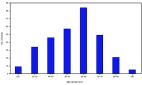
The mean of the estimated differences between the proportion of cases and proportion
of the population consisting of each underrepresented racial/ethnic group in all counties
with disparities ranged from 4.5% (NHPI) to 39.3% (AI/AN) (Table 3). The mean of the
estimated ratio of the proportion of cases to the proportions of population were also
generated for each underrepresented racial/ethnic group and ranged from 2.3 (black)
to 8.5 (NHPI).
TABLE 3
Proportion of cumulative COVID-19 cases compared with proportion of population in
79 counties identified as hotspots during June 5–18, 2020 with racial/ethnic disparities*
— 22 states February–June 2020
Racial/Ethnic group
Mean of estimated differences, † % (range)
Mean of estimated ratios of proportion of cases to proportion of population§ (range)
Hispanic/Latino
30.2 (8.0–68.2)
4.4 (1.2–14.6)
Black/African American
14.5 (2.3–31.7)
2.3 (1.2–7.0)
American Indian/Alaska Native
39.3 (16.4–57.9)
4.2 (1.9–6.4)
Asian
4.7 (2.7–6.8)
2.9 (2.0–4.7)
Native Hawaiian/Other Pacific Islander
4.5 (0.1–31.5)
8.5 (2.7–18.4)
Abbreviation: COVID-19 = coronavirus disease 2019.
* Disparities were defined as percentage
difference of ≥5% between the proportion of cases and the proportion of the population
or a ratio ≥1.5 for the proportion of cases to the proportion of the population) for
underrepresented racial/ethnic groups in each county.
† The mean of the estimated differences between the proportion of cases in a given
racial/ethnic group and the proportion of persons in that racial/ethnic group in the
overall population among all counties with disparities identified by the analysis.
For example, if Hispanic/Latino persons make up 20% of the population in a given county
and 30% of the cases in that county, then the difference would be 10% and the county
is considered to have a disparity.
§ The ratio of the estimated proportion of cases to the proportion of population for
each racial/ethnic group among all counties with disparities identified by the analysis.
For example, if American Indian/Alaskan Native persons made up 0.5% of the population
in a given county and 1.5% of the cases in that county, then the ratio of proportions
would be 3.0, and the county is considered to have a disparity.
Discussion
These findings illustrate the disproportionate incidence of COVID-19 among communities
of color, as has been shown by other studies, and suggest that a high percentage of
cases in hotspot counties are among persons of color (
1
–
5
,
7
). Among all underrepresented racial/ethnic groups in these hotspot counties, Hispanic
persons were the largest group living in hotspot counties with a disparity in cases
identified within that population (3.5 million persons). This finding is consistent
with other evidence highlighting the disproportionate incidence of COVID-19 among
the Hispanic population (
2
,
7
). The disproportionate incidence of COVID-19 among black populations is well documented
(
1
–
3
). The findings from this analysis align with other data indicating that black persons
are overrepresented among COVID-19 cases, associated hospitalizations, and deaths
in the United States. The analysis found few counties with disparities among AI/AN
populations. This finding is likely attributable to the smaller proportions of cases
and populations of AI/AN identified in hotspot counties, as well as challenges with
data for this group, including a lack of surveillance data and misclassification problems
in large data sets.
¶
Asian populations were disproportionately affected by COVID-19 in a small number of
hotspot counties. Few studies have assessed COVID-19 disparities among Asian populations
in the United States.** The Asian racial category is broad, and further subgroup analyses
might provide additional insights regarding the incidence of COVID-19 in this population.
Disparities in COVID-19 cases in NHPI populations were identified in nearly one quarter
of hotspot counties. For some hotspot counties with small NHPI populations, this finding
might be related, in part, to the analytic methodology used. Using a ratio of ≥1.5
in the proportion of population and proportion of cases to indicate disparities is
sensitive to small differences in these groups. More complete county-level race/ethnicity
data are needed to fully evaluate the disproportionate incidence of COVID-19 among
communities of color.
Disparities in COVID-19–associated mortality in hotspot counties were not assessed
because the available county-level mortality data disaggregated by race/ethnicity
were not sufficient to generate reliable estimates. Existing national analyses highlight
disparities in mortality associated with COVID-19; similar patterns are likely to
exist at the county level (
5
). As more complete data are made available in the future, county-level analyses examining
disparities in mortality might be possible. COVID-19 disparities among underrepresented
racial/ethnic groups likely result from a multitude of conditions that lead to increased
risk for exposure to SARS-CoV-2, including structural factors, such as economic and
housing policies and the built environment,
††
and social factors such as essential worker employment status requiring in-person
work (e.g., meatpacking, agriculture, service, and health care), residence in multigenerational
and multifamily households, and overrepresentation in congregate living environments
with an increased risk for transmission (
4
,
7
–
9
). Further, long-standing discrimination and social inequities might contribute to
factors that increase risk for severe disease and death, such as limited access to
health care, underlying medical conditions, and higher levels of exposure to pollution
and environmental hazards
§§
(
4
). The conditions contributing to disparities likely vary widely within and among
groups, depending on location and other contextual factors.
Rates of SARS-CoV-2 transmission vary by region and time, resulting in nonuniform
disease outbreak patterns across the United States. Therefore, using epidemiologic
indicators to identify hotspot counties currently affected by SARS-CoV-2 transmission
can inform a data-driven emergency response. Tailoring strategies to control SARS-CoV-2
transmission could reduce the overall incidence of COVID-19 in communities. Using
these data to identify disproportionately affected groups at the county level can
guide the allocation of resources, development of culturally and linguistically tailored
prevention activities, and implementation of focused testing efforts.
The findings in this report are subject to at least five limitations. First, more
than half of the hotspot counties did not report sufficient race data and were therefore
excluded from the analysis. In addition, many hotspot counties included in the analyses
were missing data on race for a significant proportion of cases (mean = 28.3%; range
= 2.6%–48.7%). These data gaps might result from jurisdictions having to reconcile
data from multiple sources for a large volume of cases while data collection and management
processes are rapidly evolving.
¶¶
Second, health departments differ in the way race/ethnicity are reported, making comparisons
across counties and states more difficult. Third, differences in how race/ethnicity
data are collected (e.g., self-report versus observation) likely varies by setting
and could lead to miscategorization. Fourth, differences in access to COVID-19 testing
could lead to underestimates of prevalence in some underrepresented racial/ethnic
populations. Finally, the number of cases that had available race/ethnicity data for
the period of study of hotspots (June 5–18) was too small to generate reliable estimates,
so cumulative case counts by county during February–June 2020 were used to identify
disparities. This approach describes the racial/ethnic breakdown of cumulative cases
only. Therefore, these data might not provide an accurate estimate of disparities
during June 5–18, which could be under- or overestimated, or change over time.
Developing culturally responsive, targeted interventions in partnership with trusted
leaders and community-based organizations within communities of color might reduce
disparities in COVID-19 incidence. Increasing the proportion of cases for which race/ethnicity
data are collected and reported can help inform efforts in the short-term to better
understand patterns of incidence and mortality. Existing health inequities amplified
by COVID-19 highlight the need for continued investment in communities of color to
address social determinants of health*** and structural racism that affect health
beyond this pandemic (
4
,
8
). Long-term efforts should focus on addressing societal factors that contribute to
broader health disparities across communities of color.
Summary
What is already known about this topic?
Long-standing health and social inequities have resulted in increased risk for infection,
severe illness, and death from COVID-19 among communities of color.
What is added by this report?
Among 79 counties identified as hotspots during June 5–18, 2020 that also had sufficient
data on race, a disproportionate number of COVID-19 cases among underrepresented racial/ethnic
groups occurred in almost all areas during February–June 2020.
What are the implications for public health practice?
Identifying health disparities in COVID-19 hotspot counties can inform testing and
prevention efforts. Addressing the pandemic’s disproportionate incidence among communities
of color can improve community-wide health outcomes related to COVID-19.
Related collections
Most cited references6

- Record: found
- Abstract: found
- Article: found
Coronavirus Disease 2019 Case Surveillance — United States, January 22–May 30, 2020
Erin K. Stokes, Laura Zambrano, Kayla N. Anderson … (2020)
- Record: found
- Abstract: found
- Article: found
Characteristics and Clinical Outcomes of Adult Patients Hospitalized with COVID-19 — Georgia, March 2020
Jeremy Gold, Karen Wong, Christine Szablewski … (2020)

- Record: found
- Abstract: found
- Article: found
Characteristics Associated with Hospitalization Among Patients with COVID-19 — Metropolitan Atlanta, Georgia, March–April 2020
Marie Killerby, Ruth Link-Gelles, Sarah Haight … (2020)