- Record: found
- Abstract: found
- Article: found
Successful entecavir plus prednisolone treatment for hepatitis B virus-associated membranoproliferative glomerulonephritis : A case report
Read this article at
Abstract
Rationale:
Adult-onset hepatitis B virus-associated membranoproliferative glomerulonephritis (HBV-MPGN) is generally refractory, and an effective treatment for this condition has not been established. The indications for steroids in HBV-MPGN are an important clinical concern.
Patient concerns:
A 28-year-old woman with a chronic hepatitis B virus infection developed nephrotic syndrome in her second month of pregnancy, with urinary protein levels of 3 to 10 g/d that continued into her postpartum period. She was a carrier of HBV with HBeAg seroconversion. As her renal impairment could have been a result of pregnancy, we observed her for 10 months postpartum without any intervention. However, spontaneous remission after childbirth was not achieved and urine protein levels were sustained at 1 to 3 g/d. About 10 months after delivery, elevated serum liver enzyme levels were observed.
Diagnosis:
Biopsies showed MPGN, with deposition of hepatitis B antigen in the glomeruli, and chronic B-type hepatitis with a severity grade of A1F0. She was diagnosed with HBV-MPGN.
Interventions:
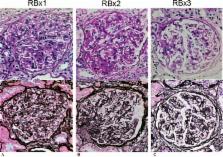
The patient was started on entecavir 0.5 mg/d in March 2008. Within 1 month, serum HBV DNA became undetectable; within 3 months, her alanine aminotransferase levels normalized. However, urinary protein excretion did not decrease to <2 g/d. On a second renal biopsy, performed 7 months after entecavir treatment, proliferative lesions of the glomeruli were observed; therefore, prednisolone was started at an initial dose of 30 mg/d.
Outcomes:
Her proteinuria improved immediately and prednisolone was tapered over 10 months. A third renal biopsy showed a remarkable resolution of HBV-MPGN, with a significant decrease in mesangial proliferation and immune complex deposition. HBV reactivation was not observed during the prednisolone treatment.
Related collections
Most cited references21
- Record: found
- Abstract: not found
- Article: not found
Hepatitis B cure: From discovery to regulatory approval
- Record: found
- Abstract: found
- Article: not found