- Record: found
- Abstract: found
- Article: found
Kirschner wire versus external fixation in the treatment of proximal humeral fractures in older children and adolescents: a comparative study

Read this article at
Abstract
Objective
The purpose of this study was to compare the therapeutic effects of Kirschner wire fixation and external fixation in the treatment of proximal humeral fractures in older children and adolescents.
Methods
A retrospective analysis was performed on the clinical data of older children and adolescents who underwent surgery at our institution for proximal humeral fractures between April 2014 and May 2022. One group (n = 28) underwent fracture reduction and Kirschner wire fixation, and the other group (n = 23) underwent external fixation. During the follow-up, the differences in shoulder joint function between the two groups were compared by analysing Quick Disabilities of the Arm, Shoulder, and Hand (Quick DASH) and Constant-Murley scores. Postoperative complications were also recorded.
Results
The operation time of the Kirschner wire group was shorter than that of the external fixation group (69.07 ± 11.34 min vs. 77.39 ± 15.74 min, P = 0.33). The time to remove the fixator in the external fixation group was shorter than that in the Kirschner wire group (6.74 ± 1.57 vs. 7.61 ± 1.22, P = 0.032). The Quick DASH score and Constant-Murley score of the patients in the external fixation group were significantly better than those in the Kirschner wire group at 3 months after surgery (5.63 ± 4.33 vs. 8.93 ± 6.40, P = 0.040; 93.78 ± 2.43 vs. 91.75 ± 2.15, P = 0.003). There was no significant difference in the Quick DASH score or Constant-Murley score between the patients in the external fixator group and those in the Kirschner wire group at 9 months after the operation (2.77 ± 3.14 vs. 3.17 ± 3.68, P = 0.683; 97.39 ± 1.80 vs. 96.57 ± 2.15, P = 0.152). The most common complication of the two groups was pin tract infection. The incidence rate of infection was higher in the external fixation group than that in the Kirschner wire group (9 vs. 4, P = 0.043).
Conclusion
Both Kirschner wire fixation and external fixation of N-H III and IV proximal humeral fractures in older children and adolescents produce good outcomes. External fixation is a preferred surgical treatment option for paediatric proximal humerus fractures because early mobilization of the affected limb can be realized.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Proximal humerus fractures in the pediatric population: a systematic review
- Record: found
- Abstract: found
- Article: found
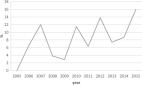
The incidence and treatment trends of pediatric proximal humerus fractures

- Record: found
- Abstract: found
- Article: found