- Record: found
- Abstract: found
- Article: found
Magnitude of Reduction and Speed of Remission of Suicidality for Low Amplitude Seizure Therapy (LAP-ST) Compared to Standard Right Unilateral Electroconvulsive Therapy: A Pilot Double-Blinded Randomized Clinical Trial
Read this article at
Abstract
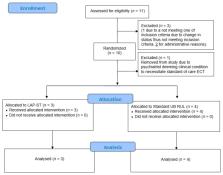
Background: Although treatment guidelines support use of electroconvulsive therapy (ECT) for acute suicidality, it is associated with cognitive side effects. The effect of Low Amplitude Seizure Therapy (LAP-ST) on suicidality is unknown. Our prior precision LAP-ST (pLAP-ST) performing titrating in the current domain has provided initial proof of concept data in humans of its advantage in terms of reduction of cognitive side effects. The aims of this report are to: 1) compare LAP-ST (at 500mA) versus standard Right Unilateral (RUL) ECT (at 900 mA) in terms of magnitude of remission of suicidality in a randomized allocation and 2) compare the speed of remission of suicidality between LAP-ST versus RUL ECT. Methods: Patients were randomized to either LAP-ST or RUL ECT. The scores pertaining to the suicidal ideation (SI) item on the Montgomery-Åsberg Depression Rating Scale (MADRS) were analyzed using descriptive analysis and no confirmatory statistical analysis was performed due to a priori sample size limitations for this pilot study. SI item remission was defined as 2 or below on this item. Results: Eleven patients with major depressive episode (MDE) of mainly unipolar or bipolar disorders signed consent. Of these, 7 were eligible and were randomized and included in the analysis; all were actively suicidal at baseline (suicide item above 2), except 1 patient who had suicide item at 2 in the RUL ECT group. Suicidality remitted on average by session 3 and remission occurred for all patients by session 4. The SI mean score improvement from baseline to endpoint for LAP-ST was 5.1 and for RUL ECT was 3.0. Conclusions: LAP-ST has larger effect size and speed of remission of suicidality compared to standard RUL ECT. Future studies are warranted for replicating these findings. (ClinicalTrials.gov ID: NCT02583490).
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: found
Treatment-resistant depression: therapeutic trends, challenges, and future directions
- Record: found
- Abstract: found
- Article: not found
A review of the clinical, economic, and societal burden of treatment-resistant depression: 1996-2013.

- Record: found
- Abstract: found
- Article: found