- Record: found
- Abstract: found
- Article: found
Increased Epicardial Adipose Tissue Is Associated with the Airway Dominant Phenotype of Chronic Obstructive Pulmonary Disease
Read this article at
Abstract
Background
Epicardial adipose tissue (EAT) has been shown to be a non-invasive marker that predicts the progression of cardiovascular disease (CVD). It has been reported that the EAT volume is increased in patients with chronic obstructive pulmonary disease (COPD). However, little is known about which phenotypes of COPD are associated with increased EAT.
Methods
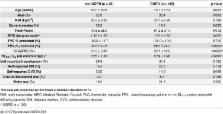
One hundred and eighty smokers who were referred to the clinic were consecutively enrolled. A chest CT was used for the quantification of the emphysematous lesions, airway lesions, and EAT. These lesions were assessed as the percentage of low attenuation volume (LAV%), the square root of airway wall area of a hypothetical airway with an internal perimeter of 10 mm (√Aaw at Pi10) and the EAT area, respectively. The same measurements were made on 225 Vietnamese COPD patients to replicate the results.
Results
Twenty-six of the referred patients did not have COPD, while 105 were diagnosed as having COPD based on a FEV 1/FVC<0.70. The EAT area was significantly associated with age, BMI, FEV 1 (%predicted), FEV 1/FVC, self-reported hypertension, self-reported CVD, statin use, LAV%, and √Aaw at Pi10 in COPD patients. The multiple regression analyses showed that only BMI, self-reported CVD and √Aaw at Pi10 were independently associated with the EAT area (R 2 = 0.51, p<0.0001). These results were replicated in the Vietnamese population.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
NIH Image to ImageJ: 25 years of image analysis.
- Record: found
- Abstract: found
- Article: not found
Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study.
- Record: found
- Abstract: found
- Article: not found