- Record: found
- Abstract: found
- Article: found
Magnitude of Neural Tube Defects and Associated Risk Factors at Three Teaching Hospitals in Addis Ababa, Ethiopia
Read this article at
Abstract
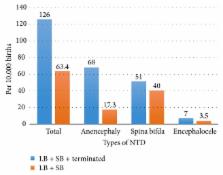
There is scarcity of data on prevalence of neural tube defects (NTDs) in lower-income countries. Local data are important to understand the real burden of the problem and explore risk factors to design and implement preventive approaches. This study aimed to determine prevalence and risk factors of NTDs. A hospital-based cross-sectional and unmatched case-control study was conducted at three teaching hospitals of Addis Ababa University. NTDs were defined as cases of anencephaly, spina bifida, and encephalocele based on ICD-10 criteria. The prevalence of NTDs was calculated per 10,000 births for both birth and total prevalence. During seven months, we observed 55 cases of NTDs out of 8677 births after 28 weeks of gestation—birth prevalence of 63.4 per 10,000 births (95% confidence interval (CI), 51–77). A total of 115 cases were medically terminated after 12 weeks of gestation. Fifty-six of these terminations (48.7%) were due to NTDs. Thus, total prevalence of NTDs after 12 weeks' gestation is 126 per 10,000 births (95% CI, 100–150). Planned pregnancy (adjusted odds ratio (aOR), 0.47; 95% CI, 0.24–0.92), male sex (aOR, 0.56; 95% CI, 0.33–0.94), normal or underweight body mass index (aOR, 0.49; 95%, 0.29–0.95), and taking folic acid or multivitamins during first trimester (aOR, 0.47; 95%, 0.23–0.95) were protective of NTDs. However, annual cash family income less than $1,300 USD (aOR, 2.5; 95%, 1.2–5.5), $1,300–1,800 USD (aOR, 2.8; 95%, 1.3–5.8), and $1,801–2,700 USD (aOR, 2.6; 95%, 1.2–5.8) was found to be risk factors compared to income greater than $2,700 USD. The prevalence of NTDs was found to be high in this setting. Comprehensive preventive strategies focused on identified risk factors should be urgently established. More studies on prevention strategies, including folic acid supplementations, should be conducted in the setting.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Effects and safety of periconceptional oral folate supplementation for preventing birth defects
- Record: found
- Abstract: found
- Article: not found
Maternal obesity and risk of neural tube defects: a metaanalysis.
- Record: found
- Abstract: found
- Article: not found