- Record: found
- Abstract: found
- Article: found
The association of reproductive hormones, thyroid function, and vitamin levels with premature ejaculation: A prospective case-control study
Read this article at
Abstract
Purpose
To investigate whether serum hormone (testosterone, prolactin, gonadotropins, and thyroid hormones) and vitamin (vitamin B 12, folic acid, and vitamin D) levels are associated with premature ejaculation (PE).
Materials and Methods
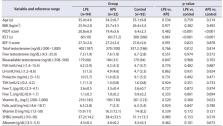
This prospective case-control study included 126 patients with PE (lifelong PE [LPE] in 94 and acquired PE [APE] in 32) who presented to the urology outpatient clinic between April 2016 and January 2023 and 92 healthy men as a control group. The diagnosis of PE was based on the criteria defined by the International Society for Sexual Medicine. Serum total testosterone (TT), free and bioavailable testosterone, follicle-stimulating hormone, luteinizing hormone, prolactin, thyroid-stimulating hormone, free triiodothyronine, thyroxine (fT 4), vitamin B 12, folic acid, and vitamin D levels were measured.
Results
Serum TT, fT 4, and vitamin D levels were significantly higher in patients with PE than in the control group (p=0.022, p=0.002, and p=0.044, respectively). However, the serum vitamin B 12 level was significantly lower in the PE group (p=0.021). In the multivariate logistic regression analysis, only vitamin B 12 was found to be an independent risk factor for PE, with an estimated odds ratio of 0.997 (95% confidence interval 0.994–0.999, p=0.036).
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction.
- Record: found
- Abstract: found
- Article: not found
A critical evaluation of simple methods for the estimation of free testosterone in serum.
- Record: found
- Abstract: found
- Article: not found