- Record: found
- Abstract: found
- Article: not found
Forecasting the incidence of tuberculosis in China using the seasonal auto-regressive integrated moving average (SARIMA) model
Read this article at
Abstract
Objectives
The aims of this study were to develop a forecasting model for the incidence of tuberculosis (TB) and analyze the seasonality of infections in China; and to provide a useful tool for formulating intervention programs and allocating medical resources.
Methods
Data for the monthly incidence of TB from January 2004 to December 2015 were obtained from the National Scientific Data Sharing Platform for Population and Health (China). The Box–Jenkins method was applied to fit a seasonal auto-regressive integrated moving average (SARIMA) model to forecast the incidence of TB over the subsequent six months.
Results
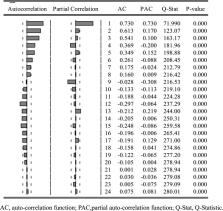
During the study period of 144 months, 12,321,559 TB cases were reported in China, with an average monthly incidence of 6.4426 per 100,000 of the population. The monthly incidence of TB showed a clear 12-month cycle, and a seasonality with two peaks occurring in January and March and a trough in December. The best-fit model was SARIMA (1,0,0)(0,1,1) 12, which demonstrated adequate information extraction (white noise test, p > 0.05). Based on the analysis, the incidence of TB from January to June 2016 were 6.6335, 4.7208, 5.8193, 5.5474, 5.2202 and 4.9156 per 100,000 of the population, respectively.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Tuberculosis prevalence in China, 1990-2010; a longitudinal analysis of national survey data.
- Record: found
- Abstract: found
- Article: not found
