- Record: found
- Abstract: found
- Article: found
Pregnancy Outcomes and Appropriate Timing of Pregnancy in 183 pregnancies in Korean Patients with SLE
Read this article at
Abstract
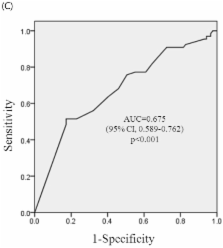
This study was undertaken to investigate the pregnancy outcomes in patients with systemic lupus erythematosus (SLE) and the appropriate timing of pregnancy. We performed a retrospective evaluation of 183 pregnancies with SLE at Catholic University Medical Center during the 13-year period from 1998 to 2010. Pregnancy outcomes were compared according to SLE characteristics. The predictive value of the different cut-off points of the stable period before conception on adverse pregnancy outcomes was calculated by ROC (Receiver operating characteristics) curve analysis. In multivariate analysis, the presence of antiphospholipid antibodies (aPLs) increased the risk of pregnancy loss (p<0.0001) and premature birth (p=0.0040). Active disease at conception increased the risk of premature birth (p< 0.0001) and complications (IUGR, PIH, or both) (p= 0.0078). The other predictor of complications was found to be lupus flare (p=0.0252). At a cut-off level of stable period of 4 months before conception, sensitivity and specificity were 70.8% and 53.2%, 71.4% and 61.5%, and 63.6 % and 59.8 %, respectively on reducing pregnancy loss, premature birth, and complications. Pregnancies with aPLs, active disease at conception and SLE flares are at a higher risk of adverse outcomes. It is essential that disease activity remains stable at least 4 months before conception, for favorable pregnancy outcomes.
Related collections
Most cited references19
- Record: found
- Abstract: not found
- Article: not found
Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus.
- Record: found
- Abstract: found
- Article: not found
A systematic review and meta-analysis of pregnancy outcomes in patients with systemic lupus erythematosus and lupus nephritis.
- Record: found
- Abstract: found
- Article: not found