- Record: found
- Abstract: found
- Article: found
Robotic versus laparoscopic ventral hernia repair: multicenter, blinded randomized controlled trial
Read this article at
Abstract
Objective
To determine whether robotic ventral hernia repair is associated with fewer days in the hospital 90 days after surgery compared with laparoscopic repair.
Participants
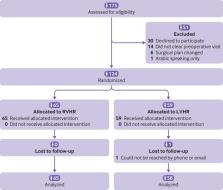
124 patients, deemed appropriate candidates for elective minimally invasive ventral hernia repair, consecutively presenting from April 2018 to February 2019.
Interventions
Robotic ventral hernia repair (n=65) versus laparoscopic ventral hernia repair (n=59).
Main outcome measures
The primary outcome was number of days in hospital within 90 days after surgery. Secondary outcomes included emergency department visits, operating room time, wound complications, hernia recurrence, reoperation, abdominal wall quality of life, and costs from the healthcare system perspective. Outcomes were pre-specified before data collection began and analyzed as intention to treat.
Results
Patients from both groups were similar at baseline. Ninety day follow-up was completed in 123 (99%) patients. No evidence was seen of a difference in days in hospital between the two groups (median 0 v 0 days; relative rate 0.90, 95% confidence interval 0.37 to 2.19; P=0.82). For secondary outcomes, no differences were noted in emergency department visits, wound complications, hernia recurrence, or reoperation. However, robotic repair had longer operative duration (141 v 77 min; mean difference 62.89, 45.75 to 80.01; P≤0.001) and increased healthcare costs ($15 865 (£12 746; €14 125) v $12 955; cost ratio 1.21, 1.07 to 1.38; adjusted absolute cost difference $2767, $910 to $4626; P=0.004). Among patients with robotic ventral hernia repair, two had an enterotomy compared none with laparoscopic repair. The median one month postoperative improvement in abdominal wall quality of life was 3 with robotic ventral hernia repair compared with 15 following laparoscopic repair.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Methods for analyzing health care utilization and costs.
- Record: found
- Abstract: found
- Article: not found
Ventral Hernia Management: Expert Consensus Guided by Systematic Review.

- Record: found
- Abstract: found
- Article: found