- Record: found
- Abstract: found
- Article: found
Systematic review of clinical guidelines for lipid lowering in the secondary prevention of cardiovascular disease events
Read this article at
Abstract
Background
The WHO recommends that those with established cardiovascular disease should be treated with lipid-lowering therapy, but there is no specific guidance regarding lipid monitoring. Unnecessary general practitioner visits may be a burden for patients and increase healthcare costs. A systematic review of the current guidelines was performed to reveal gaps in the evidence base for optimal lipid monitoring approaches.
Methods
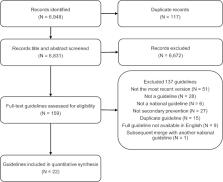
For this systematic review, a search of Medline, Cumulative Index to Nursing and Allied Health Literature and Turning Research Into Practice databases was conducted for relevant guidelines published in the 10 years prior to 31 December 2019. Recommendations surrounding the frequency of testing, lipid-lowering therapies and target cholesterol values were compared qualitatively. Each guideline was assessed using the 2009 Appraisal of Guidelines for Research and Evaluation II tool.
Results
Twenty-two guidelines were included. All recommended statins as the primary lipid-lowering therapy, with a high level of supporting evidence. Considerable variation was found in the recommendations for cholesterol targets. Seventeen guidelines provided at least one cholesterol target, which for low-density lipoprotein (LDL) cholesterol ranged between 1.0 and 2.6 mmol/L, although the most frequently recommended was <1.8 mmol/L (n=12). For long-term follow-up, many recommended reviewing patients annually (n=9), although there was some variation in recommendations for the interval of between 3 and 12 months. Supporting evidence for any approach was limited, often being derived from clinical opinion.
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease
- Record: found
- Abstract: not found
- Article: not found
AGREE II: advancing guideline development, reporting and evaluation in health care.

- Record: found
- Abstract: found
- Article: found