- Record: found
- Abstract: found
- Article: found
Radiation-Induced Secondary Cancer Risk Assessment in Patients With Lung Cancer After Stereotactic Body Radiotherapy Using the CyberKnife M6 System With Lung-Optimized Treatment
Read this article at
Abstract
Background
To evaluate the lifetime secondary cancer risk (SCR) of stereotactic body radiotherapy (SBRT) using the CyberKnife (CK) M6 system with a lung-optimized treatment (LOT) module for lung cancer patients.
Methods
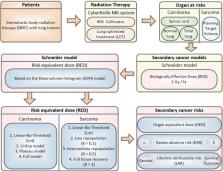
We retrospectively enrolled 11 lung cancer patients curatively treated with SBRT using the CK M6 robotic radiosurgery system. The planning treatment volume (PTV) and common organs at risk (OARs) for SCR analysis included the spinal cord, total lung, and healthy normal lung tissue (total lung volume - PTV). Schneider’s full model was used to calculate SCR according to the concept of organ equivalent dose (OED).
Results
CK-LOT-SBRT delivers precisely targeted radiation doses to lung cancers and achieves good PTV coverage and conformal dose distribution, thus posing limited SCR to surrounding tissues. The three OARs had similar risk equivalent dose (RED) values among four different models. However, for the PTV, differences in RED values were observed among the models. The cumulative excess absolute risk (EAR) value for the normal lung, spinal cord, and PTV was 70.47 (per 10,000 person-years). Schneider’s Lnt model seemed to overestimate the EAR/lifetime attributable risk (LAR).
Conclusion
For lung cancer patients treated with CK-LOT optimized with the Monte Carlo algorithm, the SCR might be lower. Younger patients had a greater SCR, although the dose–response relationship seemed be non-linear for the investigated organs, especially with respect to the PTV. Despite the etiological association, the SCR after CK-LOT-SBRT for carcinoma and sarcoma, is low, but not equal to zero. Further research is required to understand and to show the lung SBRT SCR comparisons and differences across different modalities with motion management strategies.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
Hypofractionated stereotactic radiotherapy (HypoFXSRT) for stage I non-small cell lung cancer: updated results of 257 patients in a Japanese multi-institutional study.
- Record: found
- Abstract: found
- Article: not found
Clinical outcomes of a phase I/II study of 48 Gy of stereotactic body radiotherapy in 4 fractions for primary lung cancer using a stereotactic body frame.
- Record: found
- Abstract: found
- Article: not found