- Record: found
- Abstract: found
- Article: found
Open versus minimally invasive TLIF: literature review and meta-analysis
Read this article at
Abstract
Objective
The aim of this study is to provide a comparative analysis of open vs. minimally invasive TLIF using a literature review and a meta-analysis.
Summary of background data
Lumbar interbody fusion is a well-established surgical procedure for treating several spinal disorders. Transforaminal lumbar interbody fusion (TLIF) was initially introduced in the early 1980s. To reduce approach-related morbidity associated with traditional open TLIF (OTLIF), minimally invasive TLIF (MITLIF) was developed. We aimed to provide a comparative analysis of open vs. minimally invasive TLIF using a literature review.
Methods
We searched the online database PubMed (2005–2017), which yielded an initial 194 studies. We first searched the articles’ abstracts. Based on our inclusion criteria, we excluded 162 studies and included 32 studies: 18 prospective, 13 retrospective, and a single randomized controlled trial. Operative time, blood loss, length of hospital stay, radiation exposure time, complication rate, and pain scores (visual analogue scale, Oswestry Disability Index) for both techniques were recorded and presented as means. We then performed a meta-analysis.
Results
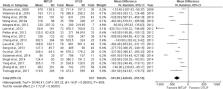
The meta-analysis for all outcomes showed reduced blood loss ( P < 0.00001) and length of hospital stay ( P < 0.00001) for MITLIF compared with OTLIF, but with increased radiation exposure time with MITLIF ( P < 0.00001). There was no significant difference in operative time between techniques ( P = 0.78). The complication rate was lower with MITLIF (11.3%) vs. OTLIF (14.2%), but not statistically significantly different ( P = 0.05). No significant differences were found in visual analogue scores (back and leg) and Oswestry Disability Index scores between techniques, at the final follow-up.
Conclusion
MITLIF and OTLIF provide equivalent long-term clinical outcomes. MITLIF had less tissue injury, blood loss, and length of hospital stay. MITLIF is also a safe alternative in obese patients and, in experienced hands, can also be used safely in select cases of spondylodiscitis even with epidural abscess. MITLIF is also a cost-saving procedure associated with reduced hospital and social costs. Long-term studies are required to better evaluate controversial items such as operative time.
Related collections
Most cited references43
- Record: found
- Abstract: found
- Article: not found
[A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author's transl)].
- Record: found
- Abstract: found
- Article: not found
Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion.
- Record: found
- Abstract: found
- Article: not found