- Record: found
- Abstract: found
- Article: found
Defining the noninferiority margin and analysing noninferiority: An overview
Read this article at
Abstract
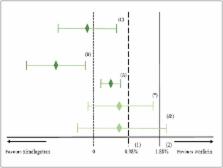
Noninferiority trials are used to assess whether the effect of a new drug is not worse than an active comparator by more than a noninferiority margin. If the difference between the new drug and the active comparator does not exceed this prespecified margin, noninferiority can be concluded. This margin must be specified based on clinical and statistical reasoning; however, it is considered as one of the most challenging steps in the design of noninferiority trials. Regulators recommend that the margin should be defined based on the historical evidence of the active comparator (the latter is often the well‐established standard treatment of the disease), which can be performed by different approaches. There are several factors and assumptions that need to be accounted for during the process of defining the margin and during the analysis of noninferiority. Three methods are commonly used to analyse noninferiority trials: the fixed‐margin method; the point‐estimate method; and the synthesis method. This article provides an overview of analysing noninferiority and choosing the noninferiority margin.
Related collections
Most cited references20
- Record: found
- Abstract: found
- Article: not found
Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke.
- Record: found
- Abstract: found
- Article: not found
Ximelagatran vs warfarin for stroke prevention in patients with nonvalvular atrial fibrillation: a randomized trial.
- Record: found
- Abstract: found
- Article: not found