- Record: found
- Abstract: found
- Article: not found
Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study
Read this article at
Summary
Background
Artemisinin-resistant falciparum malaria has arisen in western Cambodia. A concerted international effort is underway to contain artemisinin-resistant Plasmodium falciparum, but containment strategies are dependent on whether resistance has emerged elsewhere. We aimed to establish whether artemisinin resistance has spread or emerged on the Thailand–Myanmar (Burma) border.
Methods
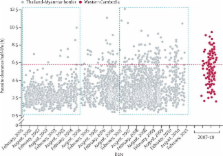
In malaria clinics located along the northwestern border of Thailand, we measured six hourly parasite counts in patients with uncomplicated hyperparasitaemic falciparum malaria (≥4% infected red blood cells) who had been given various oral artesunate-containing regimens since 2001. Parasite clearance half-lives were estimated and parasites were genotyped for 93 single nucleotide polymorphisms.
Findings
3202 patients were studied between 2001 and 2010. Parasite clearance half-lives lengthened from a geometric mean of 2·6 h (95% CI 2·5–2·7) in 2001, to 3·7 h (3·6–3·8) in 2010, compared with a mean of 5·5 h (5·2–5·9) in 119 patients in western Cambodia measured between 2007 and 2010. The proportion of slow-clearing infections (half-life ≥6·2 h) increased from 0·6% in 2001, to 20% in 2010, compared with 42% in western Cambodia between 2007 and 2010. Of 1583 infections genotyped, 148 multilocus parasite genotypes were identified, each of which infected between two and 13 patients. The proportion of variation in parasite clearance attributable to parasite genetics increased from 30% between 2001 and 2004, to 66% between 2007 and 2010.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
Qinghaosu (artemisinin): the price of success.
- Record: found
- Abstract: found
- Article: not found
Intercontinental spread of pyrimethamine-resistant malaria.
- Record: found
- Abstract: found
- Article: not found
