- Record: found
- Abstract: found
- Article: found
Risk factors for intensive care unit readmission after lung transplantation: a retrospective cohort study
Read this article at
Abstract
Background
Lung transplantation (LT) is an accepted therapeutic modality for end-stage lung disease patients. Intensive care unit (ICU) readmission is a risk factor for mortality after LT, for which consistent risk factors have not been elucidated. Thus, we investigated the risk factors for ICU readmission during index hospitalization after LT, particularly regarding the posttransplant condition of LT patients.
Methods
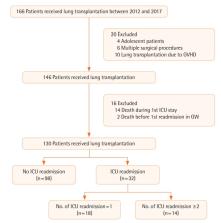
In this retrospective study, we investigated all adult patients undergoing LT between October 2012 and August 2017 at our institution. We collected perioperative data from electronic medical records such as demographics, comorbidities, laboratory findings, ICU readmission, and in-hospital mortality.
Results
We analyzed data for 130 patients. Thirty-two patients (24.6%) were readmitted to the ICU 47 times during index hospitalization. At the initial ICU discharge, the Sequential Organ Failure Assessment (SOFA) score (odds ratio [OR], 1.464; 95% confidence interval [CI], 1.083−1.978; P=0.013) and pH (OR, 0.884; 95% CI, 0.813−0.962; P=0.004; when the pH value increases by 0.01) were related to ICU readmission using multivariable regression analysis and were still significant after adjusting for confounding factors. Thirteen patients (10%) died during the hospitalization period, and the number of ICU readmissions was a significant risk factor for in-hospital mortality. The most common causes of ICU readmission and in-hospital mortality were infection-related.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: found
The SOFA score—development, utility and challenges of accurate assessment in clinical trials
- Record: found
- Abstract: found
- Article: not found
Patients readmitted to ICUs* : a systematic review of risk factors and outcomes.
- Record: found
- Abstract: not found
- Article: not found