- Record: found
- Abstract: found
- Article: found
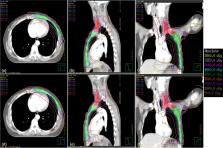
A dosimetric and radiobiological evaluation of VMAT following mastectomy for patients with left-sided breast cancer
Read this article at
Abstract
Background
To compare the dosimetric, normal tissue complication probability (NTCP), secondary cancer complication probabilities (SCCP), and excess absolute risk (EAR) differences of volumetric modulated arc therapy (VMAT) and intensity-modulated radiation therapy (IMRT) for left-sided breast cancer after mastectomy.
Methods and materials
Thirty patients with left-sided breast cancer treated with post-mastectomy radiation therapy (PMRT) were randomly enrolled in this study. Both IMRT and VMAT treatment plans were created for each patient. Planning target volume (PTV) doses for the chest wall and internal mammary nodes, PTV1, and PTV of the supraclavicular nodes, PTV2, of 50 Gy were prescribed in 25 fractions. The plans were evaluated based on PTV1 and PTV2 coverage, homogeneity index (HI), conformity index, conformity number (CN), dose to organs at risk, NTCP, SCCP, EAR, number of monitors units, and beam delivery time.
Results
VMAT resulted in more homogeneous chest wall coverage than did IMRT. The percent volume of PTV1 that received the prescribed dose of VMRT and IMRT was 95.9 ± 1.2% and 94.5 ± 1.6%, respectively ( p < 0.001). The HI was 0.11 ± 0.01 for VMAT and 0.12 ± 0.02 for IMRT, respectively ( p = 0.001). The VMAT plan had better conformity (CN: 0.84 ± 0.02 vs. 0.78 ± 0.04, p < 0.001) in PTV compared with IMRT. As opposed to IMRT plans, VMAT delivered a lower mean dose to the ipsilateral lung (11.5 Gy vs 12.6 Gy) and heart (5.2 Gy vs 6.0 Gy) and significantly reduced the V 5, V 10, V 20, V 30, and V 40 of the ipsilateral lung and heart; only the differences in V 5 of the ipsilateral lung did not reach statistical significance ( p = 0.409). Although the volume of the ipsilateral lung and heart encompassed by the 2.5 Gy isodose line (V 2.5) was increased by 6.7% and 7.7% ( p < 0.001, p = 0.002), the NTCP was decreased by 0.8% and 0.6%, and SCCP and EAR were decreased by 1.9% and 0.1% for the ipsilateral lung. No significant differences were observed in the contralateral lung/breast V 2.5, V 5, V 10, V 20, mean dose, SCCP, and EAR. Finally, VMAT reduced the number of monitor units by 31.5% and the treatment time by 71.4%, as compared with IMRT.
Conclusions
Compared with IMRT, VMAT is the optimal technique for PMRT patients with left-sided breast cancer due to better target coverage, a lower dose delivered, NTCP, SCCP, and EAR to the ipsilateral lung and heart, similar doses delivered to the contralateral lung and breast, fewer monitor units and a shorter delivery time.
Related collections
Most cited references44
- Record: found
- Abstract: found
- Article: not found
Risk of Ischemic Heart Disease in Women after Radiotherapy for Breast Cancer
- Record: found
- Abstract: found
- Article: not found
Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials.
- Record: found
- Abstract: found
- Article: not found