- Record: found
- Abstract: found
- Article: found
Hyponatremia and Worsening Sodium Levels Are Associated With Long‐Term Outcome in Patients Hospitalized for Acute Heart Failure
Read this article at
Abstract
Background
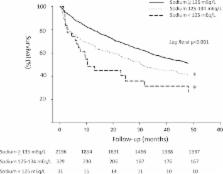
Hyponatremia predicts poor prognosis in patients with acute heart failure ( AHF). However, the association of the severity of hyponatremia and changes of serum sodium levels with long‐term outcome has not been delineated.
Methods and Results
The study population was drawn from the HARVEST registry ( Heart F ailure Registry of Taipei Veteran s General Hospi tal), so that patients hospitalized for acute heart failure ( AHF) composed this study. The National Death Registry was linked to identify the clinical outcomes of all‐cause mortality and cardiovascular death, with a follow‐up duration of up to 4 years. Among a total of 2556 patients (76.4 years of age, 67% men), 360 had on‐admission hyponatremia, defined as a serum sodium level of <135 mEq/L on the first day of hospitalization. On‐admission hyponatremia was a predictor for all‐cause mortality (hazard ratio and 95% CI: 1.43, 1.11–1.83) and cardiovascular mortality (1.50, 1.04–2.17), independent of age, sex, hematocrit, estimated glomerular filtration rate, left ventricular ejection fraction, and prescribed medications. Subjects with severe hyponatremia (<125 mEq/L) would even have worse clinical outcomes. During hospitalization, a drop of sodium levels of >3 mEq/L was associated with a marked increase of mortality than those with minimal or no drop of sodium levels. In addition, subjects with on‐admission hyponatremia and drops of serum sodium levels during hospitalization had an incremental risk of death (2.26, 1.36–3.74), relative to those with normonatremia at admission and no treatment‐related drop of serum sodium level in the fully adjusted model.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Survival after the onset of congestive heart failure in Framingham Heart Study subjects.
- Record: found
- Abstract: found
- Article: not found
Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials.
- Record: found
- Abstract: found
- Article: not found