- Record: found
- Abstract: found
- Article: found
Unmet health care needs of older people: prevalence and predictors in a French cross-sectional survey
Read this article at
Abstract
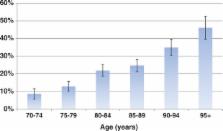
Background: Unmet health care needs are associated with negative health outcomes, yet there is a paucity of data on this problem among older people. Objective: To identify unmet health care needs and associated factors among older people in France. Methods: This is a cross-sectional population study of people aged 70 years or older in which 2350 respondents were interviewed in 2008–10. During a standardized interview, a nurse examined health problems, functional abilities and use of health care resources. Unmet health care needs were defined as situations in which a participant needed health care and did not receive it. Results: The mean age was 83.2 ± 7.4 years. Almost all participants reporting a chronic disease (98.6%) had consulted a physician in the previous 6 months. Unmet health care needs were found in 23.0% of the sample and mainly consisted of lack of dental care (prevalence of 17.7%), followed by lack of management of visual or hearing impairments (prevalence of 4.4% and 3.1%, respectively). Age was the main factor associated with unmet health care needs [compared with people aged 70–79: odds ratio 80–89 years = 2.26 (1.70–3.03), odds ratio 90 years and over = 3.85 (2.71–5.45)]. Other associated factors were regular smoking, homebound status, poor socioeconomic conditions, depression, limitations in instrumental activities of daily living and low medical density. Conclusion: Unmet health care needs affect almost one-quarter of older people in France. Efforts should be made to improve oral health and develop home care, especially for the oldest-olds.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Development and validation of a geriatric depression screening scale: a preliminary report.
- Record: found
- Abstract: found
- Article: not found
Inequalities in access to medical care by income in developed countries.
- Record: found
- Abstract: found
- Article: not found