- Record: found
- Abstract: found
- Article: found
Efficacy and Safety of Ertugliflozin in Patients with Overweight and Obesity with Type 2 Diabetes Mellitus
Read this article at
Abstract
Objective
This study aimed to evaluate ertugliflozin in patients with overweight and obesity with type 2 diabetes mellitus.
Methods
Data from three placebo‐controlled, randomized, Phase 3 studies were pooled. Patients with baseline BMI ≥ 25 (1,377/1,544; 89%) were assessed with a stratification by BMI subgroup.
Results
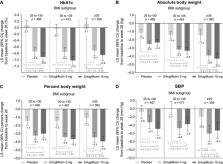
At week 26, reductions from baseline in glycated hemoglobin A1c (HbA1c), fasting plasma glucose, body weight (BW), and systolic blood pressure (SBP) were greater with ertugliflozin versus placebo. For placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively, least squares mean change was 0.1%, −0.8%, and −0.9% for HbA1c and −1.2 kg, −3.1 kg, and −3.2 kg for BW. HbA1c reductions were consistent across BMI subgroups. For ertugliflozin 5 mg and 15 mg, least squares mean change (placebo adjusted) in absolute BW was −1.4 kg and −1.2 kg for BMI 25 to < 30, −1.8 kg and −1.9 kg for BMI 30 to < 35, and −2.5 kg and −2.9 kg for BMI ≥ 35. Percent BW changes were similar across BMI subgroups. Incidence of adverse events was 52.5%, 44.6%, and 50.1% with placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively.
Conclusions
Meaningful reductions in HbA1c, fasting plasma glucose, BW, and SBP were observed with ertugliflozin in patients with overweight and obesity with type 2 diabetes mellitus. Ertugliflozin improved HbA1c and SBP and reduced BW across BMI subgroups. Ertugliflozin was generally well tolerated.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Sodium Glucose Cotransporter 2 Inhibitors in the Treatment of Diabetes Mellitus: Cardiovascular and Kidney Effects, Potential Mechanisms, and Clinical Applications.
- Record: found
- Abstract: found
- Article: not found
Efficacy and safety of sodium-glucose co-transporter-2 inhibitors in type 2 diabetes mellitus: systematic review and network meta-analysis
- Record: found
- Abstract: found
- Article: not found