- Record: found
- Abstract: found
- Article: found
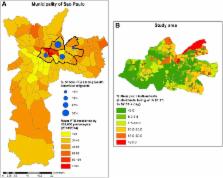
Migration and tuberculosis transmission in a middle-income country: a cross-sectional study in a central area of São Paulo, Brazil
Read this article at
Abstract
Background
Little is known about the impact of growing migration on the pattern of tuberculosis (TB) transmission in middle-income countries. We estimated TB recent transmission and its associated factors and investigated the presence of cross-transmission between South American migrants and Brazilians.
Methods
We studied a convenient sample of cases of people with pulmonary TB in a central area of São Paulo, Brazil, diagnosed between 2013 and 2014. Cases with similar restriction fragment length polymorphism (IS 6110-RFLP) patterns of their Mycobacterium tuberculosis complex isolates were grouped in clusters (recent transmission). Clusters with both Brazilian and South American migrants were considered mixed (cross-transmission). Risk factors for recent transmission were studied using logistic regression.
Results
Isolates from 347 cases were included, 76.7% from Brazilians and 23.3% from South American migrants. Fifty clusters were identified, which included 43% South American migrants and 60.2% Brazilians (odds ratio = 0.50, 95% confidence interval = 0.30–0.83). Twelve cross-transmission clusters were identified, involving 24.6% of all clustered cases and 13.8% of all genotyped cases, with migrants accounting for either an equal part or fewer cases in 11/12 mixed clusters.
Conclusions
Our results suggest that TB disease following recent transmission is more common among Brazilians, especially among those belonging to high-risk groups, such as drug users. Cross-transmission between migrants and Brazilians was present, but we found limited contributions from migrants to Brazilians in central areas of São Paulo and vice versa.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Reinfection and mixed infection cause changing Mycobacterium tuberculosis drug-resistance patterns.
- Record: found
- Abstract: found
- Article: not found
Risk factors associated with recent transmission of tuberculosis: systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found