- Record: found
- Abstract: found
- Article: found
Subclinical hypothyroidism and the risk of chronic kidney disease in T2D subjects : A case-control and dose-response analysis
Read this article at
Abstract
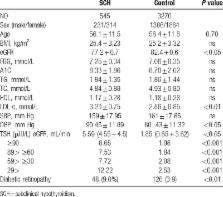
Evidence indicated a positive association between subclinical hypothyroidism (SCH) and cardiovascular diseases. But the relationship between SCH and chronic kidney diseases (CKD) remains unclear. A case-control study was performed to ascertain this relationship followed by a meta-analysis. In this hospital-based, case-control study, we recruited 3270 type 2 diabetic patients with euthyroidism and 545 type 2 diabetic patients with SCH. All English studies were searched upon the relationship between SCH and CKD up to October 2016. Meta-analysis was performed using STATA 13.0 software. Our case-control study indicated an association between SCH and CKD in patients with type 2 diabetes [OR (95% CI): 1.22 (1.09–1.36)]. Five observational studies reporting risk of CKD in SCH individuals were enrolled. A significant relationship between SCH and CKD was shown [pooled OR 1.80, (95% CI) 1.38–2.35]. Among normal TSH range, individuals with TSH ≥3.0 μIU/ml had a significantly higher rate of CKD (Fisher exact test, P = 0.027). Dose-response linear increase of CKD events was explored [pooled OR 1.09 (95% CI): 1.03–1.16 per1 mIU/L increase of TSH]. The present evidence suggests that SCH is probably a significant risk factor of CKD in T2D. Linear trend is shown between TSH elevation and CKD in T2D. This relationship between serum TSH and renal impairment in type 2 diabetic patients needs further studies to investigate.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
The clinical significance of subclinical thyroid dysfunction.
- Record: found
- Abstract: found
- Article: not found
Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999.
- Record: found
- Abstract: found
- Article: not found