- Record: found
- Abstract: found
- Article: found
Multiple Ligament Reconstructions of the Knee and Posterolateral Corner
Read this article at
Abstract
Injuries to the knee involving multiple ligaments occur in a variety of circumstances and require careful assessment and planning. A wide constellation of injuries can occur with causes sufficiently traumatic to produce bicruciate ligament deficiency, and this technical report will describe diagnosis, treatment and rehabilitation for a knee dislocation with lateral injury (KD-III-L on the Schenk classification). Reconstruction in the acute setting is preferred, with anatomic-based, single-bundle anterior cruciate ligament reconstruction, double-bundle posterior cruciate ligament reconstruction, and anatomic reconstruction of the posterolateral corner using two grafts for the 3 primary posterolateral corner stabilizers. Tunnel orientation to prevent convergence and sequence of graft tensioning and fixation are discussed as well. Successful outcomes have been achieved using these anatomic-based reconstruction techniques along with appropriate rehabilitation and bracing.
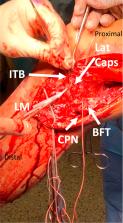
Technique Video
Repair of bicruciate ligament injury with grade III posterolateral corner tear. Examination under anesthesia is consistent with KD-III-L injury. Dissection of biceps femoris tendon (BFT) and common peroneal nerve (CPN) is performed through a lateral hockey stick incision. A fibular tunnel is drilled first, then a tibial tunnel for the popliteus tendon (PLT) and popliteofibular ligament (PLT). Femoral tunnels for the PLT and fibular collateral ligament (FCL) are drilled, oriented 35°anteromedially. Bone-patellar tendon-bone autograft is then harvested. After diagnostic arthroscopy, the PCL anterolateral bundle (ALB) and posteromedial bundle (PMB) tunnels are drilled, then the anterior cruciate ligament (ACL) femoral tunnel. A tibial guide pin is placed, confirmed with fluoroscopy, then a tunnel reamed and a large smoother passed. The ACL tibial tunnel is then reamed. The PMB graft of the PCL is passed first and secured, then the ALB. The ends of both bundles are passed down the tibial tunnel using the smoother. The ACL femoral graft is pulled into place and secured. The femoral ends of the FCL and PLT grafts are then secured. The FCL graft is passed under the iliotibial band (ITB) and through the fibular head tunnel. PCL grafts are then fixed on the anterior tibial cortex with screws and washers; ALB in 90° flexion and PMB in extension. This eliminated the posterior drawer. The ACL graft is then secured on the anterior tibia. The FCL graft is then secured in the fibular head tunnel with a screw at the anterior aperture. The PLT and PFL grafts are then passed from posterior to anterior through the tibial PLC tunnel and secured with a screw. Suture anchors are used to repair the lateral capsule and biceps femoris tendon, and the ITB repaired. Closure completes the procedure.
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: found
Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found