- Record: found
- Abstract: found
- Article: found
Current Therapeutic Strategies and Novel Approaches in Osteosarcoma
Read this article at
Abstract
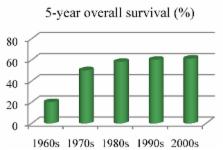
Osteosarcoma is the most frequent malignant primary bone tumor and a main cause of cancer-related death in children and adolescents. Although long-term survival in localized osteosarcoma has improved to about 60% during the 1960s and 1970s, long-term survival in both localized and metastatic osteosarcoma has stagnated in the past several decades. Thus, current conventional therapy consists of multi-agent chemotherapy, surgery and radiation, which is not fully adequate for osteosarcoma treatment. Innovative drugs and approaches are needed to further improve outcome in osteosarcoma patients. This review describes the current management of osteosarcoma as well as potential new therapies.
Related collections
Most cited references152
- Record: found
- Abstract: found
- Article: not found
Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma.
- Record: found
- Abstract: found
- Article: not found