- Record: found
- Abstract: found
- Article: found
Twelve Chinese herbal preparations for the treatment of depression or depressive symptoms in cancer patients: a systematic review and meta-analysis of randomized controlled trials
Read this article at
Abstract
Background
Patients with cancer are vulnerable to depression or other depressive conditions. The aim of this paper was to evaluate the efficacy and safety of Chinese herbal medicine (CHM) for the treatment of depression or depressive symptoms in cancer patients.
Methods
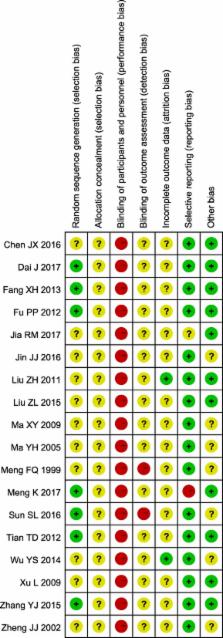
CENTRAL, MEDLINE, EMBASE, PsycINFO, CNKI, VIP, SinoMed, and online clinical trial registry websites were searched for relevant RCTs until May 2017. The methodological quality of each included study was assessed with the “risk of bias” tool. Review Manager 5.3.5 was used to analyze the data.
Results
We identified 18 RCTs that included data from 1441 participants. Twelve different types of Chinese herbal preparations were investigated by these studies, and they showed a better therapeutic effect in most comparisons when measured in terms of depression rating scale scores, with SMDs (95% CI) of − 2.30 (− 3.54, − 1.05) (CHM versus no treatment), − 0.61 (− 1.03, − 0.18) (CHM versus antidepressants), and − 0.55 (− 1.07, − 0.02) (CHM plus psychological treatments versus psychological treatments), or when measured in terms of treatment response rate, with RRs (95% CI) of 1.65 (1.19, 2.29) (CHM versus no treatment), 1.15 (1.03, 1.28) (CHM versus psychological treatments), 1.32 (1.07, 1.63) (CHM plus antidepressants versus antidepressants), and 1.70 (1.02, 2.85) (CHM plus psychological treatments versus psychological treatments). Compared with antidepressants, these CHMs showed borderline superiority for improving the response rate, with an RR (95% CI) of 1.08 (0.93, 1.26). Subgroup analysis based on psychiatric diagnosis (depression versus depressive symptoms) did not modify the direction of these estimates and neither could it explain the high level of heterogeneity. Patients in the CHM group experienced fewer adverse events of cardiac toxicity ( P = 0.02), functional gastrointestinal disorders ( P = 0.008), sleep disturbances (P = 0.02), blurred vision (P = 0.02) and fatigue ( P = 0.03) than the patients in the no treatment group or the antidepressants group.
Conclusions
According to the investigation of the twelve herbal preparations, the CHM intervention appears to alleviate depressive symptoms in cancer patients, either alone or combined with antidepressants or psychological treatments. However, a high risk of bias and high heterogeneity made the mean estimates uncertain. Well-designed trials with comprehensive and transparent reporting are warranted in the future.
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: not found
Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials.
- Record: found
- Abstract: found
- Article: not found
Association of depression and anxiety on quality of life, treatment adherence, and prognosis in patients with advanced non-small cell lung cancer.
- Record: found
- Abstract: found
- Article: not found
