- Record: found
- Abstract: found
- Article: found
Persistence of Ebola virus in various body fluids during convalescence: evidence and implications for disease transmission and control
Read this article at
SUMMARY
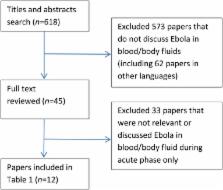
The aim of this study was to review the current evidence regarding the persistence of Ebola virus (EBOV) in various body fluids during convalescence and discuss its implication on disease transmission and control. We conducted a systematic review and searched articles from Medline and EMBASE using key words. We included studies that examined the persistence of EBOV in various body fluids during the convalescent phase. Twelve studies examined the persistence of EBOV in body fluids, with around 800 specimens tested in total. Available evidence suggests that EBOV can persist in some body fluids after clinical recovery and clearance of virus from the blood. EBOV has been isolated from semen, aqueous humor, urine and breast milk 82, 63, 26 and 15 days after onset of illness, respectively. Viral RNA has been detectable in semen (day 272), aqueous humor (day 63), sweat (day 40), urine (day 30), vaginal secretions (day 33), conjunctival fluid (day 22), faeces (day 19) and breast milk (day 17). Given high case fatality and uncertainties around the transmission characteristics, patients should be considered potentially infectious for a period of time after immediate clinical recovery. Patients and their immediate contacts should be informed about these risks. Convalescent patients may need to abstain from sex for at least 9 months or should use condoms until their semen tests are negative. Breastfeeding should be avoided during the convalescent phase. There is a need for more research on persistence, and a uniform approach to infection control guidelines in convalescence.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Ebola RNA Persistence in Semen of Ebola Virus Disease Survivors - Preliminary Report.
- Record: found
- Abstract: found
- Article: not found
Ebola haemorrhagic fever in Sudan, 1976. Report of a WHO/International Study Team.
- Record: found
- Abstract: found
- Article: not found