- Record: found
- Abstract: found
- Article: found
Venous Thromboembolism Complicated with COVID-19: What Do We Know So Far?
Read this article at
Abstract
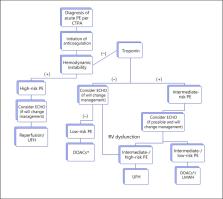
Coronavirus disease (COVID-19) is caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and is responsible for the ongoing 2019–2020 pandemic. Venous thromboembolism (VTE), a frequent cardiovascular and/or respiratory complication among hospitalized patients, is one of the known sequelae of the illness. Hospitalized COVID-19 patients are often elderly, immobile, and show signs of coagulopathy. Therefore, it is reasonable to assume a high incidence of VTE among these patients. Presently, the incidence of VTE is estimated at around 25% of patients hospitalized in the intensive care unit for COVID-19 even under anticoagulant treatment at prophylactic doses. In this review, we discuss present knowledge of the topic, the unique challenges of diagnosis and treatment of VTE, as well as some of the potential mechanisms of increased risk for VTE during the illness. Understanding the true impact of VTE on patients with COVID-19 will potentially improve our ability to reach a timely diagnosis and initiate proper treatment, mitigating the risk for this susceptible population during a complicated disease.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
Clinical Characteristics of Coronavirus Disease 2019 in China
- Record: found
- Abstract: found
- Article: not found
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
- Record: found
- Abstract: found
- Article: not found
