- Record: found
- Abstract: found
- Article: found
Mechanisms by Which Liposomes Improve Inhaled Drug Delivery for Alveolar Diseases

Read this article at
Abstract
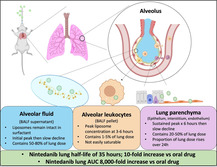
Diseases of the pulmonary alveolus, such as pulmonary fibrosis, are leading causes of morbidity and mortality, but exceedingly few drugs are developed for them. A major reason for this gap is that after inhalation, drugs are quickly whisked away from alveoli due to their high perfusion. To solve this problem, the mechanisms by which nano‐scale drug carriers dramatically improve lung pharmacokinetics using an inhalable liposome formulation containing nintedanib, an antifibrotic for pulmonary fibrosis, are studied. Direct instillation of liposomes in murine lung increases nintedanib's total lung delivery over time by 8000‐fold and lung half life by tenfold, compared to oral nintedanib. Counterintuitively, it is shown that pulmonary surfactant neither lyses nor aggregates the liposomes. Instead, each lung compartment (alveolar fluid, alveolar leukocytes, and parenchyma) elutes liposomes over 24 h, likely serving as “drug depots.” After deposition in the surfactant layer, liposomes are transferred over 3–6 h to alveolar leukocytes (which take up a surprisingly minor 1–5% of total lung dose instilled) in a nonsaturable fashion. Further, all cell layers of the lung parenchyma take up liposomes. These and other mechanisms elucidated here should guide engineering of future inhaled nanomedicine for alveolar diseases.
Abstract
Inhaled drug‐loaded liposomes reach the distal lung where they interact with alveolar fluid, leukocytes, and parenchymal cells. The liposomes are not lysed or aggregated in bronchoalveolar lavage fluid, and alveolar macrophages are not saturable. Compared to oral dosing, these intratracheally instilled liposomes deliver 8000‐fold more cargo drug to the lung with a concomitant tenfold increase in lung half life.