- Record: found
- Abstract: found
- Article: not found
The counter regulatory axis of the renin angiotensin system in the brain and ischaemic stroke: Insight from preclinical stroke studies and therapeutic potential

Read this article at
Abstract
Stroke is the 2nd leading cause of death worldwide and the leading cause of physical disability and cognitive issues. Although we have made progress in certain aspects of stroke treatment, the consequences remain substantial and new treatments are needed. Hypertension has long been recognised as a major risk factor for stroke, both haemorrhagic and ischaemic. The renin angiotensin system (RAS) plays a key role in blood pressure regulation and this, plus local expression and signalling of RAS in the brain, both support the potential for targeting this axis therapeutically in the setting of stroke. While historically, focus has been on suppressing classical RAS signalling through the angiotensin type 1 receptor (AT 1R), the identification of a counter-regulatory axis of the RAS signalling via the angiotensin type 2 receptor (AT 2R) and Mas receptor has renewed interest in targeting the RAS. This review describes RAS signalling in the brain and the potential of targeting the Mas receptor and AT 2R in preclinical models of ischaemic stroke. The animal and experimental models, and the route and timing of intervention, are considered from a translational perspective.
Related collections
Most cited references255
- Record: found
- Abstract: found
- Article: found
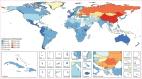
Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016
- Record: found
- Abstract: found
- Article: not found

